Innovations in Maternity Case Management
15-minute read
Health Plans Embrace an Integrated Approach to Improving Quality and Outcomes Across the Maternity Journey
This paper highlights how integrated maternity case management improves health outcomes and reduces costs by addressing medical, behavioral, and social risks throughout the maternity journey.
What you will learn:
-
How integrated care outperforms traditional maternity case management
-
Why early risk detection and personal support reduce complications
-
How combined maternity and NICU programs solve clinical issues, social determinants of health, and ensure health equity
Start Reading

Health Plans Embrace an Integrated Approach to Improving Quality and Outcomes Across the Maternity Journey
Rising Costs & Complexity: Why Health Plans Need Smarter Maternity Solutions
More than one in ten babies in the United States is born prematurely. While medical advancements have improved birth outcomes, maternal mortality and morbidity rates, as well as the cost of pregnancy and postpartum complications continue to rise.
Recognizing these challenges, health plans and employer groups are looking for innovative maternity case management solutions to improve maternal health while controlling costs.
As pregnancy and postpartum care become increasingly complex and expensive, collaboration with the right partners is crucial to supporting mothers, caregivers, families, and infants from conception through 12 months postpartum and an infant’s first year of life. Advanced solutions take a holistic, integrated approach—combining technology and personalized support to improve the member experience, enhance outcomes, and manage expenses. Leading programs blend maternity case management with digital tools, optimize NICU care management, and ensure accurate NICU payment integrity.
Maternal Morbidity & Mortality are at a Dangerous Crossroads
Maternal morbidity and mortality in the United States remain critical public health concerns, with significant racial disparities. In 2023, the overall maternal mortality rate was 18.66 deaths per 100,000 live births, more than double that of other high-income countries.
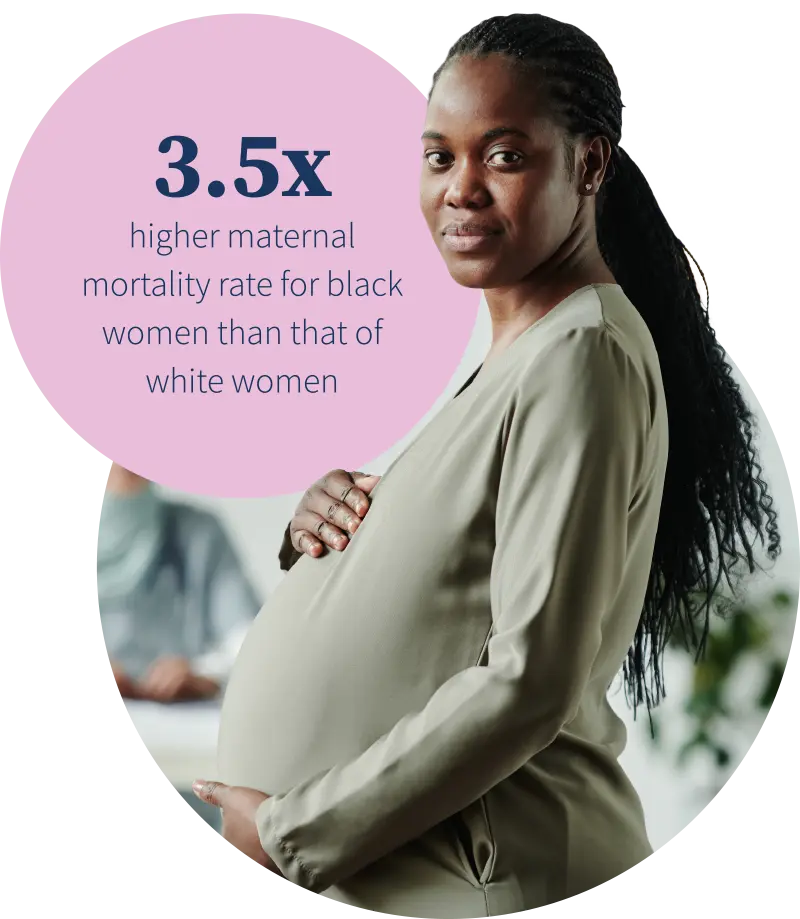
Black women continue to face disproportionately high maternal mortality rates. In 2023, the maternal mortality rate for Black women was 50.3 deaths per 100,000 live births, nearly 3.5 times higher than that of white women, whose rate declined to 14.5 per 100,000.
These statistics underscore the urgent need for comprehensive strategies to address maternal health disparities, including improved access to quality prenatal care, culturally competent healthcare practices, specialized case management, and targeted public health interventions.

Maternity Costs Keep Rising
Recent analyses indicate that preterm births and maternal morbidities continue to impose substantial economic burdens in the United States with an estimated cost of at least $25.2 billion. The last study conducted in 2020 estimated the direct per capita medical care costs of prematurity to be approximately $32,300, with the majority (85%) incurred during the first year of life.
Additionally, a 2021 report estimated total maternal morbidity costs for all U.S. births to be $32.3 billion from conception through the child’s fifth birthday, equating to $8,624 in additional costs to society for each maternal-child pair. These figures underscore the ongoing need for effective interventions to reduce preterm births and maternal health complications.
Health Plans Embrace “Full Continuum” Maternal & Infant Health Care Management Programs
Today, integrated maternity and NICU care management programs are being implemented to help payer organizations reduce the incidence and severity of premature births, improve health outcomes, and lower overall birth-related costs.
Most importantly, a dedicated maternity nurse and/or social worker builds a personal, trusted relationship with the pregnant or postpartum member to address concerns, support behavioral changes, and reduce the impact of risk factors.
“Health plans are partnering with innovators who are more proactive in managing maternity cases. They seek partners who can manage these cases holistically to drive health equity and quality outcomes for their members.”
Dr. Ellie Stang
Founder & Executive Chairwoman
The Limitations of Traditional Case Management
Early concerns slip through the cracks
Health plans have traditionally offered maternity programs for high-risk pregnancies, but low engagement and delayed identification limit their impact. Many members receive only generic pregnancy information, missing personalized support that could address rising risks.
Claims-based risk assessments – Plans identify high-risk pregnancies based solely on claims history, assuming complete member data. However, frequent plan changes and limited pre-pregnancy claims lead to under-identification. This approach also overlooks behavioral, lifestyle, and social risks, leaving many without proper support.
Apps without people – Mobile apps offer a scalable way to support low-risk pregnancies, appealing to younger, tech-savvy users. However, engagement is mixed, especially among those with SDoH challenges or health issues. While apps provide education and symptom guidance, they lack the personal support of Case Managers, who help drive app usage, address concerns, connect members to resources, and provide ongoing care, which is critical for those facing complex needs.
“When a pregnant person is unwell, struggling with food access, or needs help getting to appointments, they want a Case Manager’s support. Trained professionals are essential to preventing complications.”
Janna Lacatell
VP, Product Management
The Need for an Integrated Approach

Timely identification
Timely engagement is key to effective maternity case management, but lack of awareness and delayed claims-based identification hinder outreach. ProgenyHealth addresses this by using multiple data sources and provider referrals to identify pregnancies while proactively reaching out via phone, achieving a 70% enrollment rate among those we reach. The ProgenyHealth mobile app also allows members to enroll early, helps track symptoms, capture risk data, and educate members on having a healthy pregnancy – and this data flows back to the Case Manager for greater member insights.
Casting a wider net
Effective maternity programs reach all pregnant members early, regardless of risk, conducting ongoing, comprehensive risk assessments. Beyond claims and medical concerns, they consider home life, relationships, mental health, and lifestyle for a full picture of pregnancy risk.
“We find that even if a pregnancy is considered to be low-risk from a historical claims point of view, there may be undiscovered social or behavioral health needs that can quickly become an emergent or urgent health situation,” Janna Lacatell explained. “Suppose an individual is experiencing high stress levels during pregnancy, perhaps due to work or financial strain. This may lead to high blood pressure and a serious risk of preeclampsia or preterm birth. By casting a wider net and connecting with all pregnant people, we can be more proactive in identifying and addressing these issues. More importantly, the member has a way of reaching out, 24/7, if they have symptoms or concerns.”
Single source case management
Offering a single point for case management during the entire maternal journey reduces stress and creates an easy way for members to seek trusted support.
“Case Managers build rapport with the members, and it’s a trusted relationship. When members can confide in their nurse or social worker, we can build interventions that keep them compliant with their treatment plan.”
Madeline Szabo
SVP, Clinical Operations
Risk Assessments Deliver Value

App-Based Assessments
Traditional telephone-based risk assessments can feel inconvenient, especially for busy individuals. App-based assessments, however, can be completed anytime, anywhere. Data from the mobile app helps create a personalized profile, which can be shared with the member’s provider and the ProgenyHealth Case Manager. The level of risk also guides the frequency of Case Manager outreach.

Risk Factors for Prematurity
While the exact cause of premature birth is unknown, risk factors include previous preterm births, multiple pregnancies, substance use, and short intervals between pregnancies. Addressing complications can help prevent early delivery.

Risk is a Moving Target
Risk in pregnancy is constantly shifting due to changes in hormones, metabolism, and overall health. Because risks can emerge unpredictably, staying engaged with a support system is key to managing them. Risk assessments go beyond initial evaluations, with continuous outreach, both digital and human, helping to identify emerging risks early and guide expectant mothers to the necessary care for better outcomes.
Opportunities for Quality Improvements & Cost Savings
Improving Infant and Maternal Health Outcomes
Addressing maternal morbidities that may arise post-discharge is also crucial. Implementing case management strategies can help prevent manageable health issues from escalating into emergency situations that include ED visits and hospital readmissions.
Clinical Interventions
To reduce overall cost of birth, apps and Case Managers can educate pregnant women on recognizing signs and symptoms. Case Managers monitor preeclampsia, changes in risk level, and adhere to clinical guidelines. A holistic approach, addressing behavioral health and social determinants is also vital to success.
An often overlooked, yet critical approach to managing overall cost of birth is optimization of NICU Case Management, NICU Utilization Management, and Payment Integrity. Should a NICU admission occur, ProgenyHealth’s NICU Case Management team supports infants and their families through every milestone. Whether it’s emotional support, health literacy training, or assistance with discharge, ensuring infants are not readmitted is essential for success and a smooth transition home. Through NICU Utilization Management, ProgenyHealth ensures each NICU admission is warranted, and that each infant receives the appropriate level of care and length of stay. There is a wide variation in NICU care across hospitals, leading to disparities in treatment and outcomes. ProgenyHealth’s program goes beyond traditional Utilization and Case Management while standardizing care to optimize both clinical and financial results.
“We are moving from a strictly medical focus to behavioral health, and social determinants of health. This means treating people as a whole, which includes factors such as anxiety, diet, substance abuse, and postpartum depression.”
Linda Genen, MD, MPH
Chief Medical Officer
A Continuum of Maternity Care
Education plays a crucial role in maternity case management. Informed patients make the most of their provider visits, ensure they receive the appropriate care, and feel empowered to make care decisions. Effective maternity case management also intersects with NICU case management, if needed, to improve outcomes and reduce costs by helping to reduce and better manage a NICU admission. It further ensures continuity of care, whether for preterm births or infants requiring complex care. Timely intervention, such as addressing preterm labor or preparing families for NICU admissions, can lead to better experiences and outcomes.
Health plans are now embracing a holistic approach, offering both maternity and NICU care management programs to support mothers, infants, and providers in managing care more effectively and efficiently.
The Takeaway
Health plans, providers, and partners are working together to reduce preterm births by engaging women and birthing individuals earlier in the pregnancy journey.
Using an integrated approach – one that is backed by personalized case management, specialized expertise, and commitment to a more holistic approach, ProgenyHealth is delivering on its promise of improving the landscape of maternal, infant, and family health.
“To have a successful program that holistically manages moms and babies, you have to have a maternity and infant case management program, plus a program which supports members and providers as acute care management continues to rise. We offer the continuum of services needed today, and these services work better together. Even if a traditional health plan has a maternity case management program, they don’t necessarily have deep expertise in managing NICU cases.”
Susan Torroella, MBA
Chief Executive Officer
About ProgenyHealth
ProgenyHealth empowers our health plan and employer partners to change the trajectory of maternal and infant health outcomes across America. Informed by more than 20 years of experience and patient data, our end-to-end maternal and infant care management solution helps ensure the best possible outcomes for every expecting mother we touch. Our wholly integrated, tech-enabled solution builds a network of support for an uninterrupted continuum of care from prenatal health, through any resultant Neonatal Intensive Care Unit (NICU) stay, and all the way to one full year of life for NICU graduates and 12 months postpartum for women. From the very beginning, we unite early health risk assessment data with self-directed digital tools and dedicated Case Managers who work tirelessly to connect at-risk moms-to-be with the resources, care, and support they need for a healthier, full-term delivery. Our industry-leading intelligent platform, Baby Trax™, integrates utilization management (UM) and case management (CM), while also driving payment validation & assurance (PVA) activities based on clinical data. By promoting predictable, equitable, and standardized high-quality care journeys, we ensure healthier outcomes—and lower costs—across an entire at-risk population. In so doing, we help overcome systemic barriers to support healthier pregnancies and healthier starts to life for all moms and babies, one family at a time.



